A #missingtype repost of "The ABCs of ABO Blood Types".
If the letters A, B and O went missing in everyday life, it would be difficult to understand the world around us. When we are missing the blood groups or types that the letters A, B and O represent, it becomes difficult to treat critically ill hospital patients and save lives. Blood type is one way we are all connected and this post, originally published during National Blood Donor Week in June, digs into the science and history behind ABO.
A brief history of ABO
In the early days of transfusion medicine, doctors gave patients all sorts of different fluids, including blood or milk from animals. Success varied, and the results were often disastrous—even when they used human blood.
It wasn’t until the start of the 20th century that physicians learned the ABCs of the ABO blood types and finally understood how to give a successful transfusion.
Before learning about blood types, doctors noticed that mixing blood samples from patient and donor sometimes caused clumping, or agglutination. They also noticed that transfusion could destroy the patient’s blood cells. But they usually dismissed these findings, explaining them as a part of the illness.
In 1901, Austrian doctor Karl Landsteiner decided to find out more. When he mixed red blood cells (erythrocytes) from one person with the serum, the fluid that remains after blood clots, from another, he noticed that it didn’t always clump.
With further testing, he found he could divide people into one of three groups—A, B and O (initially called C)—according to these clumping reactions. A year later, his colleagues DeCastello and Sturli added a fourth grouping, or blood type: AB.
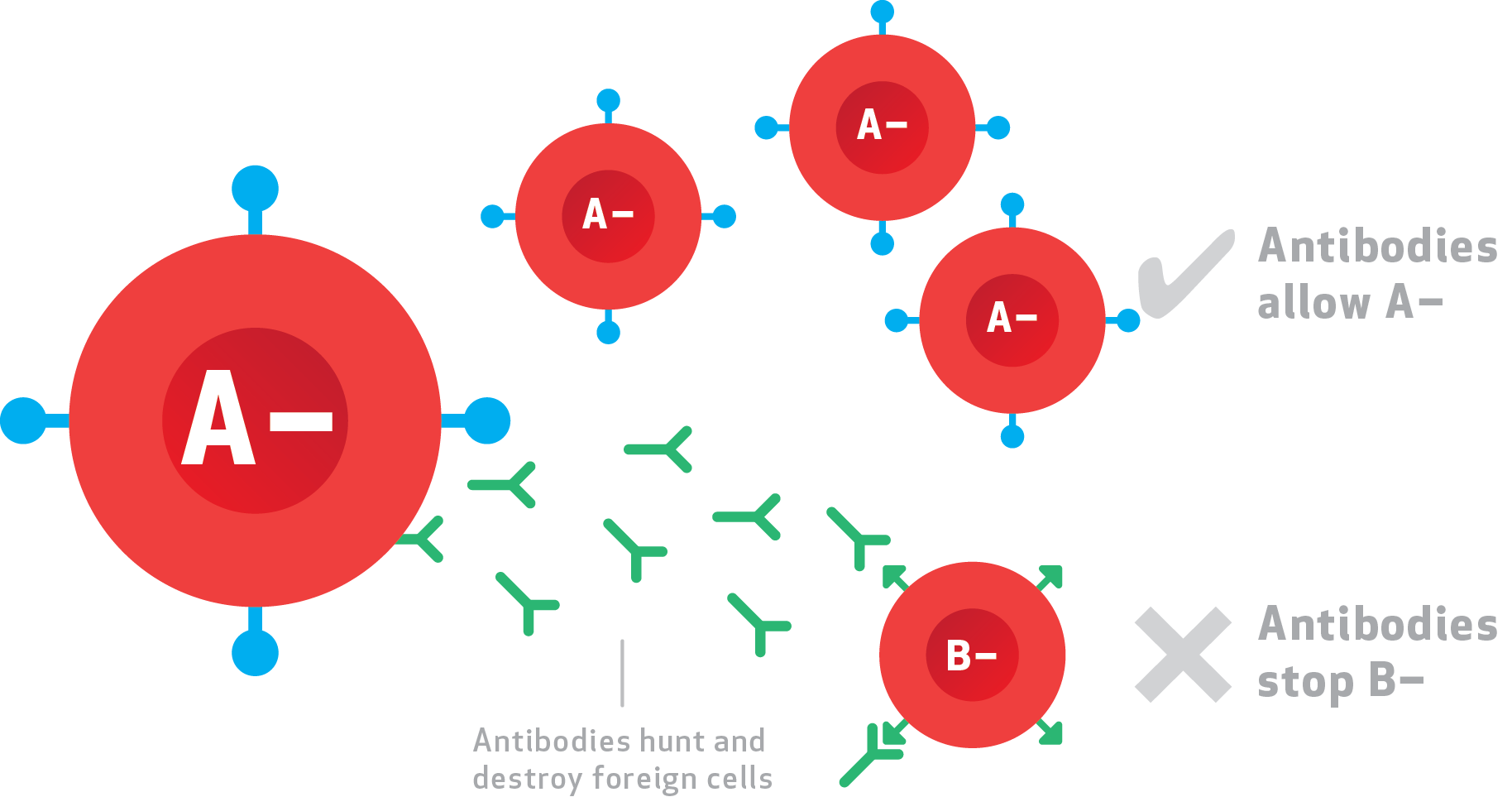
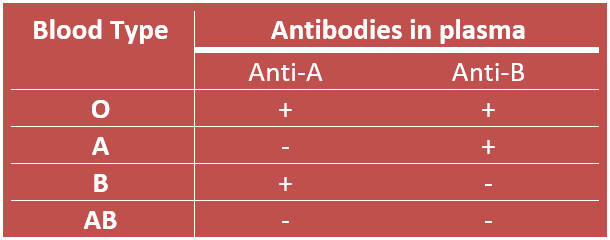
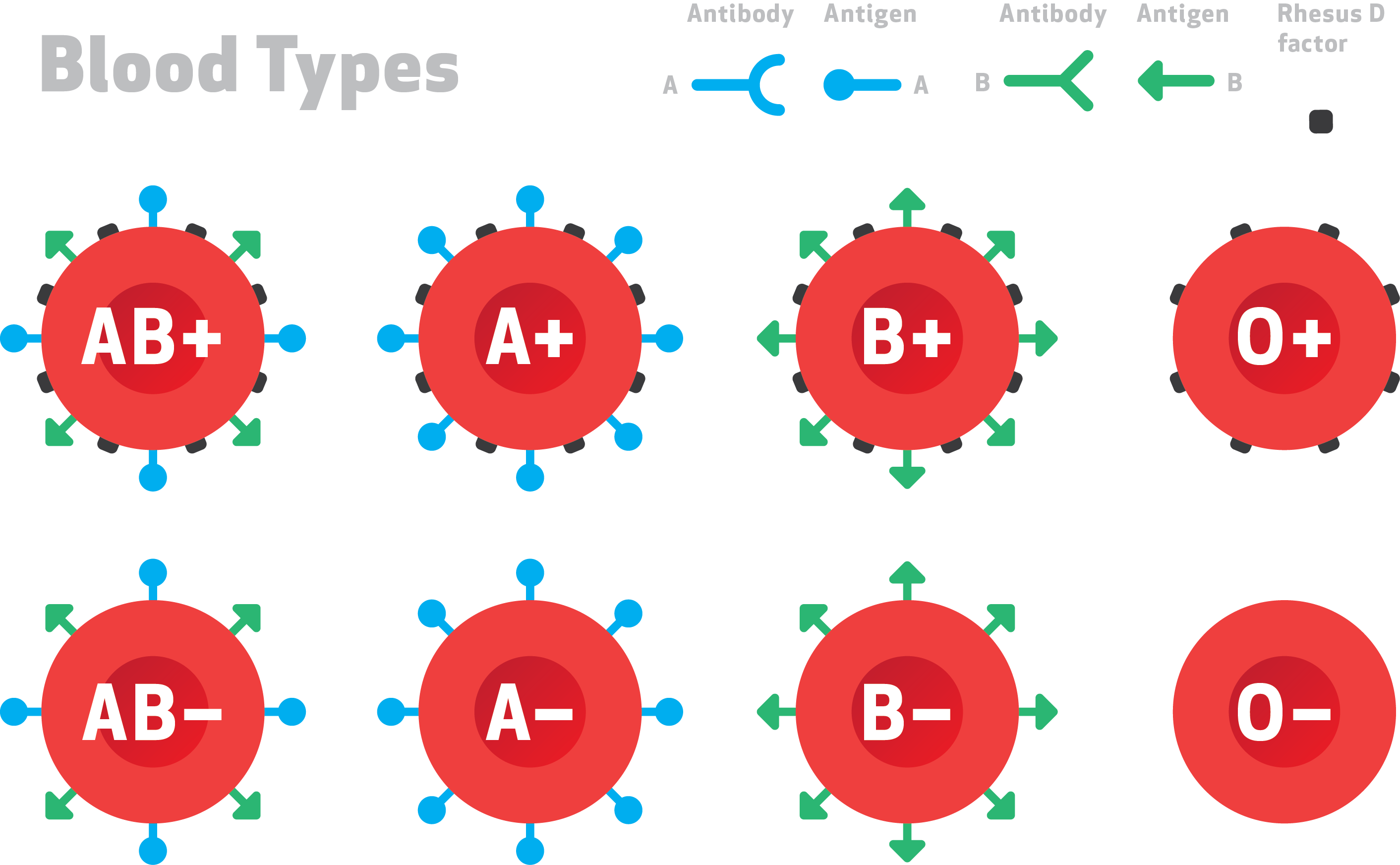
Landsteiner, with his knowledge of immunology, proposed that the agglutination was an allergic reaction. The different blood groups were caused by antigens, or surface markers on the red blood cells. People’s immune systems created antibodies, anti-A and anti-B, against the blood type they didn’t have. When different blood types were mixed together, the antibodies bound to the surface markers on the cells, making them clump together.
And Dr. Landsteiner was right. The blood type antigens are carbohydrate chains attached to glycoproteins on the red cell surface. Each of the blood types A and B carries one of two different carbohydrate chains, while type AB carries both types of chain and type O carries neither.
Furthermore, individual people make antibodies in serum against the type that they don’t carry. When red cells from a type A person are transfused into a type B person, anti-A antibodies recognize the cells as foreign and destroy them.
The same thing happens if type B blood cells are transfused into a type A person. Since type O blood does not have A or B markers, these cells can be transfused into all patients, since they they don’t cause a reaction. That’s why type O donors are described as “universal donors.” Correspondingly, type AB patients are “universal recipients”: they can receive all types of blood.
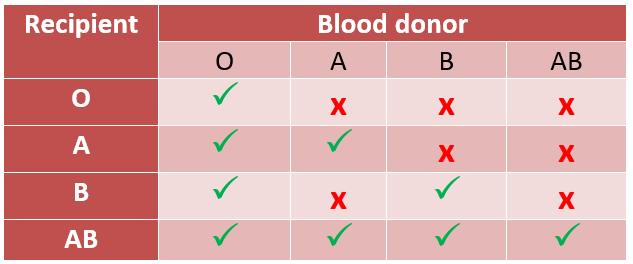
Plasma transfusions follow the opposite rules, since it is the fluid part of blood that carries the antibodies. As with red blood cells, transfusing plasma from a type A individual into a type B patient is not possible, since the anti-B antibodies would attack the recipient’s red cells—and vice versa. But type AB patients can only receive plasma from type AB donors, whereas type O patients can receive plasma from anyone.
Although ABO is the most important blood type system for transfusion medicine, clinicians need to be aware of other cell-surface antigen markers. Rhesus factor, also discovered by Landsteiner in collaboration with colleague Alexander Wiener, is a protein that spans the red cell membrane.
Most people are rhesus positive (Rh+). However, it is important to know rhesus status in transfusion medicine, especially for sensitized people and during pregnancy. In these cases, anti-rhesus antibodies will destroy red cells. During pregnancy, the antibodies cross the placenta and cause anemia in the developing child.
There are approximately 35 different blood groups in human beings, but the ABO and Rh systems are the most commonly encountered. These two are the most important in transfusion medicine. Doctors must pay attention to the ABCs of ABO by cross-matching to check for agglutination before a transfusion to make sure that the blood products will not harm the patient.
Right now, As, Bs and Os are missing in Canada. This means more people need to come forward and register their intent to donate blood this year at missingtype.ca
Further reading:
missingtype.ca
Karl Landsteiner’s 148th birthday (June 14, 2016 - Google Doodle)
Canadian Blood Services – Driving world-class innovation
Through discovery, development and applied research, Canadian Blood Services drives world-class innovation in blood transfusion, cellular therapy and transplantation—bringing clarity and insight to an increasingly complex healthcare future. Our dedicated research team and extended network of partners engage in exploratory and applied research to create new knowledge, inform and enhance best practices, contribute to the development of new services and technologies, and build capacity through training and collaboration.
The opinions reflected in this post are those of the author and do not necessarily reflect the opinions of Canadian Blood Services nor do they reflect the views of Health Canada or any other funding agency.
Related blog posts
It's National Blood Donor Week and we're celebrating blood donors from across the country who make a lifesaving difference to patients in need. Each of us has the right blood type to give life: ABOAB. This acronym refers to four blood groups — A, B, AB, and O. Blood type is one way we are all...
On that front, Canada is doing a very good job. Dr. David Allan, medical director for Canadian Blood Services’ Cord Blood Bank and OneMatch Stem Cell and Marrow Network, reports that more than 1,000 units of cord blood are now available in the public Cord Blood Bank.

