Blood processing methods affect microparticles and mtDNA linked to blood transfusion reactions
Release date: 11 April 2016
Research debunks previously held belief that storage of blood is responsible for cellular damage
OTTAWA, ON – Scientists from Blood Systems Research Institute in San Francisco, California, and Canadian Blood Services’ Centre for Innovation lab in Edmonton, Alberta, report for the first time that specific red blood cell manufacturing methods may be less damaging to cells than others. This finding could help reduce adverse reactions in transfusion recipients and may impact the future of how blood is collected in North America and around the world.
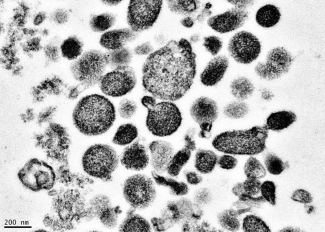
By comparing red blood cells collected at the organizations’ respective blood donation centers in the US and Canada, the researchers looked at the levels of microparticles and mitochondrial DNA (mtDNA) present in blood that can indicate cellular damage. Studying red blood cell units manufactured using nine different processes, the scientists observed clear differences in the extent of damage across the nine methods. The findings appear in Vox Sanguinis online and will be printed in an upcoming issue.
“Based on Dr. Jason Acker’s prior work, we knew that red blood cells can be damaged to varying degrees depending on the manufacturing method. We then wondered if we could detect damage-associated molecular patterns, known as DAMPs, in the red cell products, as evidenced by microparticle counts and mtDNA levels,” explains Dr. Sonia Bakkour.
Dr. Bakkour, lead researcher and staff scientist in the molecular transfusion lab at Blood Systems Research Institute, presented the team’s preliminary findings at the AABB annual meeting last October. “Our study showed that those molecular patterns are present and that their levels and composition are different based on the red cell manufacturing process, that is, the process and materials used to collect or prepare red cells for transfusion. This tells us that some manufacturing processes cause less damage to the red blood cells than others.”
“Working with the American team at Blood Systems Research Institute was key to this research because of the wide variations in blood manufacturing processes present in the US,” explains Dr. Jason Acker, senior development scientist with Canadian Blood Services’ Centre for Innovation.
“In countries like Canada, where there is a national blood service, manufacturing methods are largely standardized, so it is difficult to compare various methods. But blood collection in the US is characterized by dozens of independent blood centers that use a variety of available manufacturing processes. The Americans provided the variations we needed to measure red cell damage and to ascertain whether it can be attributed to different manufacturing methods.”
This new research also debunks the long-held belief that higher levels of DAMPs are associated with longer lengths of time red blood cell units are stored prior to transfusion. The findings show the increased levels are related to the manufacturing method, rather than the storage method. However, the researchers have not yet isolated the specific causes of the variations in mtDNA and microparticle counts.
“There must be more testing of the apheresis collections equipment, blood bags, leukoreduction filters and other variations in manufacturing methods to determine what single element or combination of elements in the various red blood cell manufacturing processes result in high levels of DAMPs and why,” emphasizes Dr. Michael Busch, senior vice president and co-director of Blood Systems Research Institute.
“We also need to understand how mitochondrial DAMPs are involved in adverse reactions to red blood cell transfusions,” elaborates Bakkour. “Some recently published studies on platelet components link high levels of mitochondrial DAMPs to adverse transfusion reactions. We need to see if DAMPs have similar adverse effects on recipients of red blood cell transfusions.”
“We think that our research could lead to finding ‘the best’ way to manufacture red blood cells,” predicts Acker. “It’s clear now that manufacturing methods matter. We and our respective research sponsors — Health Canada, US National Institutes for Health, Heart, Lung and Blood Institute are keen to explore what’s in the blood bag or in the filters or in the tubing, for example, that can be minimized or eliminated, improving the outcome in patients who receive blood transfusions.”
###
Bio of Dr. Jason Acker
Bio of Dr. Sonia Bakkour
Bio of Dr. Michael Busch
About Canadian Blood Services: Through discovery, development and applied research, Canadian Blood Services’ Centre for Innovation drives world-class innovation in blood transfusion, cellular therapy and transplantation. Canadian Blood Services manages the national supply of blood, blood products and stem cells, and related services for all the provinces and territories (excluding Quebec). We operate an integrated, pan-Canadian service delivery model that includes leading an interprovincial system for organ donation and transplantation. Our national scope, infrastructure and governance make us unique in the Canadian health-care landscape. Canadian Blood Services is regulated as a biologics manufacturer by Health Canada and primarily funded by the provincial and territorial ministries of health. We are a not-for-profit charitable organization.
For more information: (877) 709 7773, media@blood.ca or blood.ca/research.
About Blood Systems Research Institute: The Blood Systems Research Institute, based in San Francisco, is on the forefront of scientific research for transfusion-focused safety and policy issues. Funded primarily through grants and contracts, and supplemented by contributions from its Blood Systems parent organization, the institute generates and analyzes data to aid the US and worldwide transfusion medicine community by studying potential transfusion-transmitted infectious diseases and recommending donor collections and testing strategies, technology, and national and international blood banking policy.
For more information: (480) 675-5664, bkain@bloodsystems.org