Innovation150 series: As Canada celebrates 150 years we look back on Canadian innovations in transfusion medicine over the years. A series of posts over the next few weeks feature remarkable Canadian progress - past, present and future. #Innovation150.
- Part 1: Dr. Lawrence Bruce Robertson and blood transfusion in the trenches of World War I
- Part 2: Wartime Service and Canadian Transfusion Medicine
Blood-typing pioneers
Canada’s blood transfusion service and the patients who benefit from it owe a great deal to pioneering innovation in the field of blood typing. Work by immunohematologists Marie Crookston at the University of Toronto and Dr. Bruce Chown, Dr. Jack Bowman and team at the Winnipeg Rh Laboratory in the mid-twentieth century advanced clinical knowledge of transfusion reactions due to blood cell antibody responses. Their studies made the transfusion service aware of these potentially life-threatening reactions and gave clinicians new treatments. Furthermore, results like these from the broader field of blood typing also paved the way for current research looking at camouflaging blood cells and making artificial universal donor blood.
The University of Manitoba hosts an excellent look back at the history of the Winnipeg Rh Laboratory. URL: http://medheritage.lib.umanitoba.ca/?page_id=73
Dr. Bruce Chown and the Winnipeg Rh Laboratory
Dr. Bruce Chown graduated from the University of Manitoba medical school in 1922. He spent three years in pediatric research in the United States before returning to the Children’s Hospital in Winnipeg. In 1940, his research interests turned to human blood groups in general, and newborn and infant conditions in particular.
Rhesus Factor
At the time, Rhesus (Rh) factor on the surface of red blood cells and the Rh factor system were not fully understood. Although Rh factor was discovered by Karl Landsteiner in 1937, its importance became apparent only through follow-up work in 1940. A paper on hemolytic disease of newborn babies showed that this newly discovered blood type caused neonatal deaths and severe transfusion reactions.
Rh factor is a blood group antigen, a protein that spans across the red cell membrane to the outside of the cell. Humans either do or do not possess these markers, hence the blood-typing classifications Rh+ or Rh−. There are several different Rh antigens, but the most common one referred to is termed D. Normally the Rh system does not cause a problem unless an Rh− individual is sensitized and carries anti-Rh antibodies. This is rare, but sensitization can happen during pregnancy and with blood transfusion. Sensitized individuals will therefore destroy any Rh+ red blood cells they encounter.
Maternal Sensitization and Hemolytic Disease of the Newborn
Sensitization of Rh− mothers can occur during pregnancy, since fetal blood can cross the placenta and mix with the mother’s circulation, and at childbirth.
So, if an Rh− woman carries an Rh+ baby, she will create antibodies to Rh factor through alloimmunization in her first pregnancy. Although nothing happens during the first pregnancy, any further pregnancies that she has with an Rh+ partner will be affected. Quite simply, the mother’s antibodies against Rh factor cross the placental circulation to attack and destroy her developing baby’s red blood cells.
Before researchers understood this process, hundreds of families either lost or gave birth to seriously disabled babies in second and subsequent pregnancies due to erythroblastosis fetalis, or hemolytic disease of the newborn (HDN). A lot of families never had more than one child.
And this is what Chown and the Winnipeg Rh Laboratory set out to put right in 1940.
Preventing Loss and Saving Newborns
Chown and Bowman, and later Dr. Alvin Zipursky, established various protocols to save alloimmunized Rh+ newborns from hemolytic crises, disability and death.
First, with treatment, Chown initiated prompt transfusion with “clean” blood to save a newborn’s life. Chown realized that the red blood cell destruction was somehow associated with a factor in the baby’s circulation, and the exchange transfusion removed the dangerous maternal anti-Rh antibodies for protection. Along with Bowman, he pioneered even earlier transfusion, setting up the exchange treatment for the developing fetus in utero before birth.
The lab also developed early-stage testing for Rh status by examining amniotic fluid around the fetus and a proactive treatment for pregnant Rh− women using anti-Rh immunoglobulin, or anti-D. This antenatal prophylaxis, where the woman receives anti-D intramuscularly during her pregnancy, destroys fetal Rh+ cells before her immune system becomes sensitized into making her own anti-Rh antibodies and thus protects the developing fetus. Thanks to this pioneering work, Rh immune globulin (WinRho) treatment is widely available to all mothers in Canada and across the world.
Marie Crookston, Immunohematologist
At around the same time, another Canadian immunohematologist was deciphering the antigenic markers on the surface of blood cells. Marie Crookston (née Cutbush) got her Bachelor of Science degree in Melbourne, Australia, in 1946 before moving to London, United Kingdom, to work in hematology and transfusion medicine at the Medical Research Council (MRC) with Dr. P.L. Mollison.
Before marrying and moving to Canada, Crookston worked on categorizing new blood groups. In Canada, she raised a family while working in transfusion medicine at the University of Toronto, researching newborn exchange transfusion, transfusion reactions, long-term frozen blood storage and transfusion medicine.
Blood types and transfusion reactions
Blood groups ABO and Rh comprise markers sitting on the red blood cell membrane; the ABO markers are sugars, and the Rh factors are proteins. These act as antigens, sensitizing individuals who do not possess the markers into making antibodies against them. Once sensitized through exposure, the antibodies then destroy cells containing the markers by identifying them as foreign. This is benign for the host unless they are given blood of an incompatible group through transfusion or as maternal antibodies such as in HDN.
Duffy Group and hemolytic disease
Crookston and Mollison characterized a less common blood group known as the Duffy group. These glycoproteins are cell-surface receptors involved in inflammatory responses, and are found on red blood cells as well as other tissues throughout the body. Once sensitized, individuals can experience transfusion reactions from incompatible blood. Crookston characterized anti-Fya, one of the antibodies implicated in Duffy group transfusion reactions; it is also involved in a hemolytic condition in newborn babies similar to but less common than HDN.
Crookston also characterized another circulating antibody involved in transfusion reactions, anti-Lub. Although uncommon, this immune reaction also causes instances of HDN. As an assistant professor in the Department of Pathology at the University of Toronto, Crookston continued her research into immunohematology, looking at antibodies and agglutinins, which led to the development of a Rh vaccine for use during pregnancy and delivery.
Chapter 12, Hemolytic Disease of the Fetus and Newborn and Perinatal Immune Thrombocytopenia, Clinical Guide to Transfusion by Drs. Gwen Clarke and Judy Hannon (Canadian Blood Services)
Blood type basics for a universal donor?
There are many different types of blood group in existence, but the main ones that commonly cause transfusion reactions are the ABO and Rh systems. It is important for transfusion clinicians to carry out blood typing before treating patients to avoid serious reactions. However, maintaining sufficient stocks of compatible blood types is a challenge, especially for rare groups and during disasters.
Blood type O Rh− is also described as the universal donor blood, since the red blood cells do not carry A, B or RhD surface antigens. O Rh− can therefore be given to almost any patient, and blood banks try to keep high levels of it in stock. However, research into creating artificial universal donor blood is under way.
Dr. Mark Scott at the Centre for Blood Research
Dr. Mark Scott, a senior investigator with the Canadian Blood Services and the Centre for Blood Research at the University of British Columbia (UBC) is pinning camouflage to red blood cells to help them avoid a patient’s immune system. The camouflage molecule, known as PEG, sits on the cell surface and blocks antibody attack, thus protecting the donor cells from destruction. Another approach is to snip the red cell antigens from the cell membrane. UBC associate professor Dr. Jayachandran Kizhakkedathu and team have developed an enzyme that does just that, making artificial O− blood for transfusion.
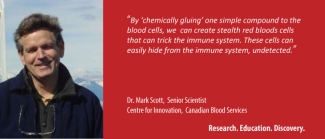
Research like this may make it possible for blood banks and transfusion services to respond quickly to patient needs in the future, serving disaster medicine where large volumes are required almost instantly, and providing safe products for patients with rare blood groups. Without pioneering basic research into blood type characterization from immunohematologists like Crookston and Chown, the idea of an artificial universal donor blood would be impossible.
This post was prepared by Amanda Maxwell, for Canadian Blood Services, with grateful thanks to Dr. Jacalyn Duffin, Queen’s University, Kingston, Ontario, for additional insights and materials.
Canadian Blood Services – Driving world-class innovation
Through discovery, development and applied research, Canadian Blood Services drives world-class innovation in blood transfusion, cellular therapy and transplantation—bringing clarity and insight to an increasingly complex healthcare future. Our dedicated research team and extended network of partners engage in exploratory and applied research to create new knowledge, inform and enhance best practices, contribute to the development of new services and technologies, and build capacity through training and collaboration. Find out more about our research impact.
The opinions reflected in this post are those of the author and do not necessarily reflect the opinions of Canadian Blood Services nor do they reflect the views of Health Canada or any other funding agency.
Related blog posts
Innovation150 series: As Canada celebrates 150 years we look back on Canadian innovations in transfusion medicine over the years. A series of posts over the next few weeks feature remarkable Canadian progress -- past, present and future. #Innovation150.
Innovation150 series on the RED blog: As Canada celebrates 150 years we look back on Canadian innovations in transfusion medicine over the years. A series of posts over the next few weeks feature remarkable Canadian progress in transfusion medicine past, present and future. #Innovation150.
![Canadian Blood Transfusion Unit which operated during the Spanish Civil War. Dr. Norman Bethune is at the right. ca. 1936 - 1938 Canadian Blood Transfusion Unit which operated during the Spanish Civil War. Dr. Norman Bethune is at the right. ca. 1936 - 1938 / Spain Source: [http://www.collectionscanada.ca/ Library and Archives Canada] Copyright: Expired](/sites/default/files/styles/max_325x325/public/Norman_Bethune_transfusion_unit_1936.png.jpeg?itok=EMjIlX_a)
![L. Bruce Robertson beside Canadian Red Cross truck, ca. [1914-1918] Copyright: Queen’s Printer for Ontario L. Bruce Robertson beside Canadian Red Cross truck, ca. [1914-1918] Copyright: Queen’s Printer for Ontario](/sites/default/files/styles/max_325x325/public/blog_images/teasers/Bruce_Robertson_beside_Canadian_Red.png.jpeg?itok=8iC6GnaS)